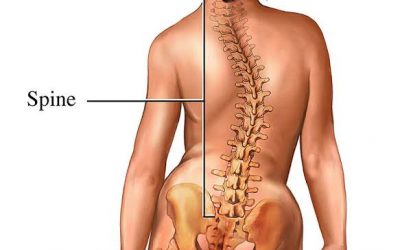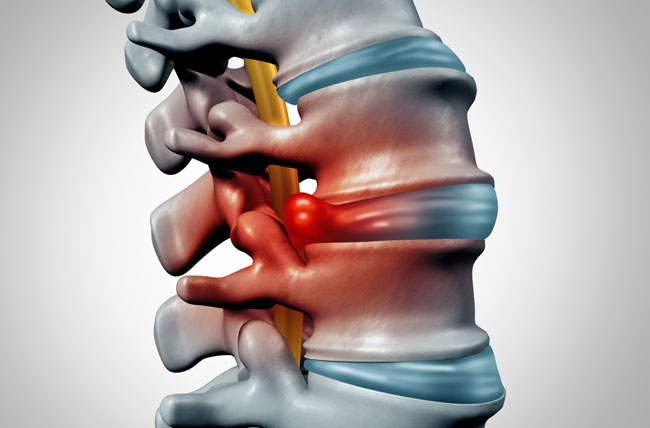
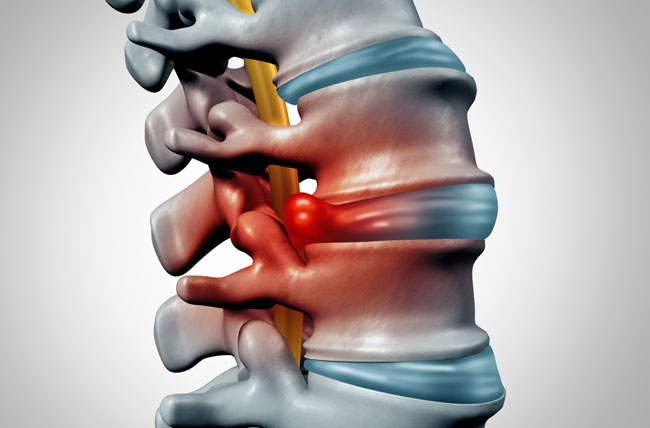
A herniated disc (also called bulged, slipped or ruptured) is a fragment of the disc nucleus that is pushed out of the annulus, into the spinal canal through a tear or rupture in the annulus.
Anatomy of herniated disk
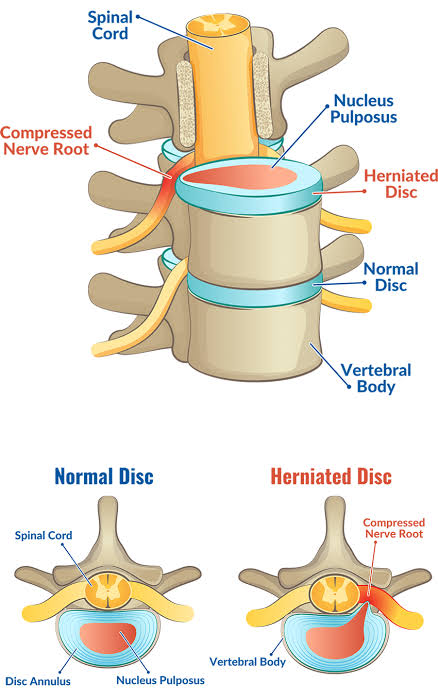
Between each vertebral body is a cushion called an intervertebral disc. Each disc absorbs the stress and shock the body incurs during movement and prevents the vertebrae from grinding against one another. The intervertebral discs are the largest structures in the body without a vascular supply. By means of osmosis, each disc absorbs needed nutrients.
Each disc is made up of two parts: the annulus fibrosus and the nucleus pulposus.
A herniated disc (also called bulged, slipped or ruptured) is a fragment of the disc nucleus that is pushed out of the annulus, into the spinal canal through a tear or rupture in the annulus. Discs that become herniated usually are in an early stage of degeneration. The spinal canal has limited space, which is inadequate for the spinal nerve and the displaced herniated disc fragment. Due to this displacement, the disc presses on spinal nerves, often producing pain, which may be severe.
Cause
A herniated disc most commonly occurs in the lower back but can also happen in the spinal column of the neck and middle back.
The cause of a herniated disk is usually gradual wear and overuse as a result of repeated movement over time. In older people, spinal disks become drier and weaker, making a herniated disk more likely.
Some medical conditions can increase the risk of disk herniation, including spinal stenosis and connective tissue disorders.
Symptoms
The pain most often occurs on one side of the body. Symptoms vary, depending on the site of injury, and may include the following:
- With a herniated disk in your lower back, you may have sharp pain in one part of the leg, hip, or buttocks, and numbness in other parts. You may also feel pain or numbness on the back of the calf or sole of the foot. The same leg may also feel weak.
- With a herniated disk in your neck, you may have pain when moving your neck, deep pain near or over the shoulder blade, or pain that moves to the upper arm, forearm, and fingers. You can also have numbness along your shoulder, elbow, forearm, and fingers.
The pain often starts slowly. It may get worse:
- After standing or sitting
- At night
- When sneezing, coughing, or laughing
- When bending backward or walking more than a few yards or meters
- When straining or holding your breath, such as when having a bowel movement
You may also have weakness in certain muscles. Sometimes, you may not notice it until your health care provider examines you. In other cases, you will notice that you have a hard time lifting your leg or arm, standing on your toes on one side, squeezing tightly with one of your hands, or other problems. Your bladder control may be lost.
The pain, numbness, or weakness often goes away or improves a lot over weeks to months.
Risk factors
Factors that can increase the risk of a herniated disk include:
- Weight. Excess body weight causes extra stress on the disks in the lower back.
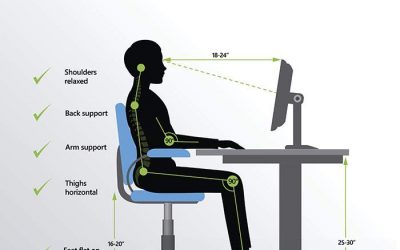
- Occupation. People with physically demanding jobs have a greater risk of back problems. Repetitive lifting, pulling, pushing, bending sideways and twisting also can increase the risk of a herniated disk.
- Genetics. Some people inherit a predisposition to developing a herniated disk.
- Smoking. It’s thought that smoking lessens the oxygen supply to disks, causing them to break down more quickly.
- Frequent driving. Being seated for long periods combined with the vibration from a motor vehicle engine can put pressure on the spine.
- Being sedentary. Regular exercise can help prevent a herniated disk.
Diagnosis
A doctor can often diagnose a herniated disk with a physical exam. They may check:
- reflexes
- the location of any painful regions in the back
- muscle strength
- range of motion
- walking ability
- sensitivity to touch
A doctor will also ask when symptoms began and whether a person has had similar symptoms in the past.
Imaging tests
In some cases, a doctor will request imaging tests. This is more likely. if the results of the physical exam indicate that there may be neurological symptoms requiring treatment.
Imaging tests include:

- CT- sacans.
- MRI scans
- X-ray scans
- discogram
- myelogram
Treatment
Keeping active and taking painkillers can help ease the pain from a slipped disc.
Keep active
If the pain is very bad, you may need to rest at first. But start gentle exercise as soon as you can – it’ll help you get better faster.
The type of exercise is not important, just gradually increase your activity level.
Take painkillers
Try anti-inflammatory painkillers such as ibuprofen to help ease the pain.
Take them regularly (up to the recommended daily amount) rather than just when the pain is particularly bad. This will help you to keep moving.
A pharmacist can help with a slipped disc
Anti-inflammatory painkillers are not suitable for everyone. Speak to a pharmacist if you’re not sure if you can take them.
You can also get advice from a pharmacist about stronger painkillers containing codeine. These can help for pain that’s just started, but they can cause addiction and should only be used for a few days.
Few people with herniated disks require surgery. If conservative treatments fail to improve your symptoms after six weeks, surgery may be an option, especially if you continue to have:
- Poorly controlled pain.
- Numbness or weakness.
- Trouble standing or walking.
- Loss of bladder or bowel control.
In nearly all cases, surgeons can remove just the protruding portion of the disk. Rarely, the entire disk must be removed. In these cases, the vertebrae might need to be fused with a bone graft.
To allow the process of bone fusion, which takes months, metal hardware is placed in the spine to provide spinal stability. Rarely, your surgeon might suggest the implantation of an artificial disk.